- Focused pricing initiatives to reduce care costs
- Efficient utilization management and unit cost management with streamlined hospital discharges and more coordinated care
- Value-based model that aligns incentives between payers and IHCS
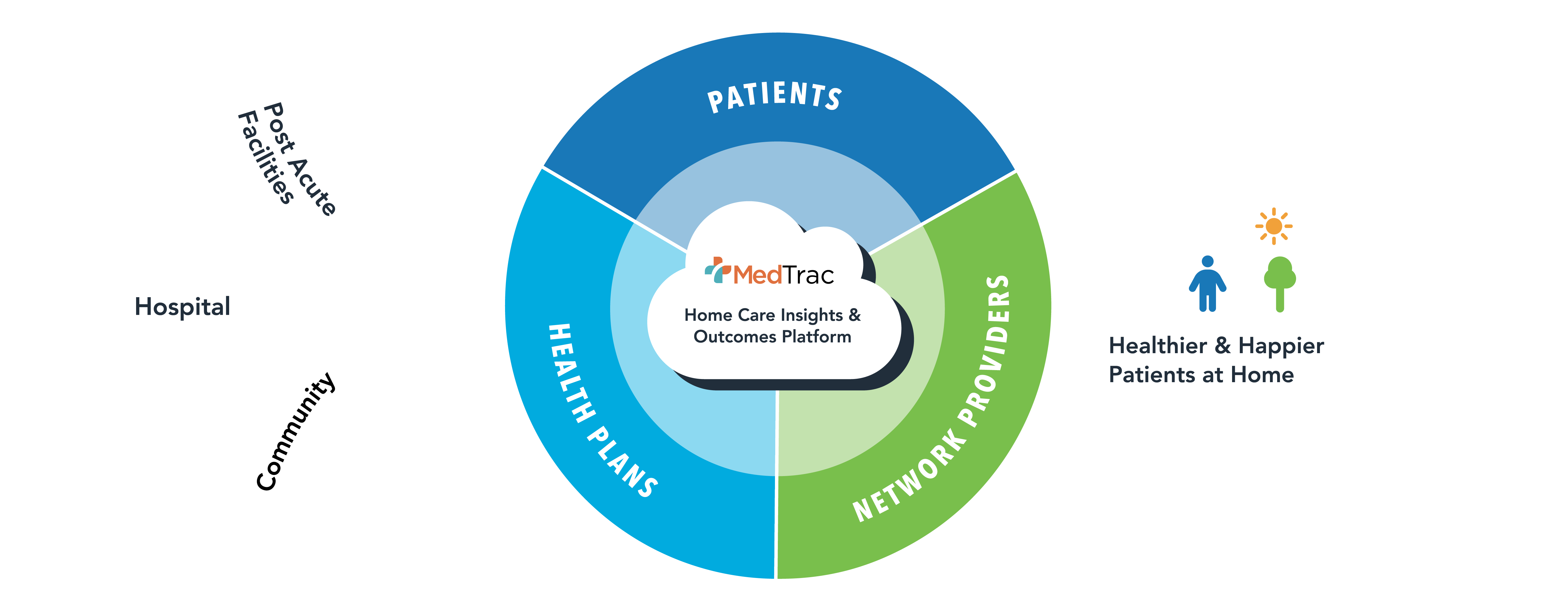
HEALTH PLANS & AT RISK PROVIDERS
Our value-based
home care model
Better, more coordinated care
at a lower cost.
Better, more coordinated care at a lower cost.
OUR BENEFITS
IHCS for Health Plans
IHCS offers a single point of contact so plan partners can easily delegate all
administrative and clinical home care functions to us. Our vertically integrated model
lowers the administrative burden, unnecessary utilization, and the total cost of care while
improving satisfaction for all stakeholders.
Home Care Benefits Management
Utilization Management
Claims Processing
& Payment
Provider Network
Credentialing & Management
Value based for
greater value
Our clinically coordinated, integrated
model enables us to put the value in
value-based care and be fully accountable
for home care program performance.
OUR BENEFITS
IHCS for At Risk Groups
We stand behind our partnership promises. IHCS is the ideal partner to help you efficiently manage and deliver optimal care and value. We stand behind our promises with performance guarantees and decades of experience managing home care without compromising quality or satisfaction.
Our customized, intentional network management model streamlines hospital discharges. With a vertically integrated model, we simplify care coordination across services. This empowers timely discharges and appropriate care transitions. Patients receive timely care and experience fewer unnecessary ER visits and readmissions.
-
- Designated member outreach to ensure appropriate and timely starts of care
- Detailed home assessments and OASIS reports that specify conditions which may lead to readmissions
- Electronic maintenance of all hospital discharge information and records for any patient taken under care post-discharge
- Medication reconciliations on all starts of care
We enable providers to streamline care and workflows to save time and reduce costs and utilization.
-
- Efficient hospital discharges and care coordination
- Streamlined credentialing processes and procedures
- Electronic claims and medical record submission
- Faster claims processing and denial notifications
Lower risk.
Higher quality.
You can’t manage care and costs without access to timely, accurate insights. IHCS gives you the immediate visibility you need, across all home care services and patient populations, to lower risk and improve care.
Claims Processing and Payment
- Claims adjudication and processing and payment of penalties in accordance with state and federal laws
- 99%+ accurate and timely processing of all claims with monthly reporting
Provider Network Credentialing & Management
- NCQA compliant
- Rigorous credentialing, auditing, and provider education
- Monthly credentialed, re-credentialed, and terminated provider reports
- FDR training and compliance oversight
- Performance, sanctions, and complaint monitoring
- Management of provider appeals process
Utilization Management
- NCQA compliant
- Referral evaluation and determination of qualifying services
- Referral assignment based on geography and clinical needs of patient
- Back-end web services with integrated address validation and real-time eligibility verification
- Built-in reporting for pending referrals and productivity management
- Turnaround reports detailing daily orders
A MODEL THAT DELIVERS
Our results speak for themselves
2
9
24
Insights
Real-time information delivery and
utilization optimization tools
Reporting
Comprehensive, real-time referral
tracking and automated reporting
Efficiencies
Optimized authorization and
claims workflows